Cervical Cancer Surgery
[/trx_title]Your gynae-oncologist will discuss your surgery with you. The type of surgery depends on the size of the cancer and whether it has spread beyond the cervix (your cancer staging will help to decide treatment).
Surgery can range from treatment which effects only the cervix such as LLETZ or cone biopsy to more radical surgery involving a hysterectomy where the uterus (womb) and cervix are removed. The ovaries and fallopian tubes may also be removed but, where possible, they are not taken out in young women as this brings on an early menopause. Lymph glands in the pelvis are also removed during a hysterectomy.
If it is necessary to remove the ovaries, the symptoms of the menopause can often be prevented by giving hormone replacement therapy (HRT) as tablets or skin patches. Your gynae-oncologist or nurse specialist will be able to discuss this with you in detail.
Cone Biopsy
This surgery involves cutting away a cone of tissue from your cervix to remove all the abnormal cells. This allows the doctor to remove a slightly larger part of the cervix than with a loop (LLETZ) biopsy. A cone biopsy also allows for the cells at the edges of the specimen to be seen clearly through a microscope ensuring that all of the biopsy can be examined be in the laboratory by the histopathologist.
A cone biopsy is usually carried out under a general anaesthetic (very small cone biopsies can be performed under local anaesthetic). The size of the cone changes according to the size of abnormal cervical cells. A vaginal pack will sometimes be put in place in theatre while you are under anaesthetic. This is like a long bandage that puts pressure on the biopsy site and so helps stop any bleeding (a bit like putting pressure on a cut to stop it bleeding). This is removed before you go home. It is advisable to have some painkillers at home (such as you would take for period pains) as some women experience a deep ache and/or tenderness in their pelvis. It is not unusual to feel tired for a few days or even a week or so following a general anaesthetic.
Large Loop Excision of the Transformational Zone (LLETZ)
Also known as LEEP or diathermy loop biopsy, this procedure uses a small wire loop and an electrical current to cut away the affected area of tissue and seal the wound at the same time. The advantage of this treatment is that the cells are removed rather than destroyed, so the tissue can be sent for further tests to confirm the extent of the cell changes and make sure the area of your cervix that contains the cells has been removed.
Trachelectomy
For some women with a very early cancer of the cervix, it may be possible to have a trachelectomy. In this type of surgery the cervix and the upper part of the vagina are removed, but the rest of the uterus (womb) is left in place. The lymph glands in the pelvis are also removed. The operation may be done as an open operation of through a combination of keyhole and vaginal surgery.
As the uterus is not removed, a trachelectomy allows for the possibility that the woman could have children. During the operation or during pregnancy, a stitch is made at the bottom of the uterus to keep it closed. There is a significantly higher chance of miscarriage or premature delivery after this procedure and the baby will be delivered early by Caesarean section [1].
Trachelectomy is only suitable for women with early stage cancer of the cervix.
This type of surgery is not common and is only done in Specialist Gynaecological Cancer Centres. You may need to ask your gynaecologist to refer you to a specialist hospital if you would like to discuss the possibility of having a trachelectomy. its important that your doctor explains the benefits and risk of this procdure.
Hysterectomy
The term ‘hysterectomy’ refers to the surgical removal of the uterus.
A hysterectomy can be advised to patients as the most appropriate treatment for conditions other than cervical cancer. A hysterectomy can be either simple or radical (sometimes called a Wertheim operation). In both cases the whole of the uterus and cervix are removed but in a radical hysterectomy the tissue at the side of the uterus, (the parametrium, and the top part of the vagina are also removed. Whether a simple or radical hysterectomy is recommended will depend on several factors including the stage and type of the tumour.
Side effects / complications after hysterectomy Some women may experience some complications after surgery and your specialist nurse or consultant will explain these complications to you.
Some women may have bladder or bowel problems after a hysterectomy because of damage to these organs (or the nerves that control them) during the surgery. This is more common after a radical operation rather than a simple hysterectomy.
If the lymph nodes have been removed, there is a risk of developing swelling (lymphoedema) in one or both legs. This is a build up of lymph fluid that cannot drain away normally because the glands have been removed. It is more likely to happen if you have had radiotherapy to the pelvic area as well as surgery.
If you develop any symptoms after your surgery, you must inform your specialist nurse or consultant as it is often possible to treat or manage them.
You may also find that after surgery, your sex life is affected. This may be as a result of the physical effects of surgery or emotional aspects of dealing with diagnosis of cancer.
If you have had your ovaries removed during the hysterectomy, you will experience early sudden menopause which produces its own symptoms, which some can find a little distressing. Do discuss this with either your GP or your nurse specialist as they can suggest options such as HRT.
Pelvic Exenteration
If, after initial treatment, your cancer comes back in the pelvic area, it may be possible to have an operation called a pelvic exenteration. This is usually only offered after chemoradiotherapy has been given. A pelvic exenteration is a major operation that involves removing all of the structures in the pelvic area and can include the womb, cervix, vagina, ovaries, bladder and the lower end of the large bowel (rectum). This type of operation is only suitable for a small number of women and you will need to have various investigations and scans to see if it is possible.
Part of the operation involves creating two openings (stomas) on the abdominal wall. These are needed because the operation removes the bladder and the rectum and you will need two stoma bags: one to collect your bowel motions and one for urine. These stomas are known as a colostomy and a urostomy. Before the operation you will see a nurse who specialises in the care of people with stomas (a stoma nurse). The nurse will explain all about stomas and how to look after them and can answer any questions you may have. The stoma nurse will also visit you after the operation to help you.
The operation usually involves making (reconstructing) a new vagina.
A pelvic exenteration is a big operation, and many women find that recovery can be difficult, both physically and emotionally. It is important that you understand exactly how the operation may affect you so it is a good idea to talk to your surgeon or specialist nurse. They can support you in deciding whether pelvic exenteration is right for you.
You may find it helpful to join our Jo’s Cervical Cancer Trusts online forum community. There are other women who have gone through pelvic exenteration who would be willing to share their stories and help support you through your surgery and recovery.
Radiotherapy
[/trx_title]Chemotherapy is not usually given as the primary treatment for cervical cancer but is often used with radiotherapy in order to make the radiotherapy more effective. You may hear this type of treatment being called chemoradiotherapy or chemoradiation. Chemotherapy makes cervical cancer more sensitive to the effects of the radiotherapy. Radiotherapy treats cancer by using high-energy rays which destroy the cancer cells, while doing as little harm as possible to normal cells. Radiotherapy for cervical cancer can be given externally or internally (Brachytherapy), and often as a combination of the two.
Radiotherapy is usually given if the cancer has spread beyond the cervix and is not curable with surgery alone. Radiotherapy may also be used after surgery if there is a high risk that the cancer may come back. It is often given in combination with chemotherapy. Your cancer specialist (clinical oncologist), who plans your treatment, will be able to discuss any concerns you may have.
Planning is a very important part of radiotherapy, and makes sure that it is as effective as possible. It may take a few visits. On your first visit to the radiotherapy department, you will be asked to have a CT scan or lie under a machine called a simulator, which takes x-rays of the area to be treated. The treatment is planned by a cancer specialist (clinical oncologist). Marks (like tiny tattoos) will be made on your skin to show the radiographer (the person who gives you your treatment) where the rays are to be directed.
External radiotherapy is usually given as an outpatient and you will need to attend every weekday (Monday – Friday) for treatment, with a rest at the weekend. This treatment will be given in the hospital radiotherapy department. High-energy x-rays are directed from a machine at the area of the cancer. The number of treatments will depend on the type and size of the cancer, but the whole course of treatment will last a few weeks. Chemotherapy is usually given once a week each week throughout the duration of your planned treatment. Your consultant or radiographer will discuss the treatment and possible side effects with you. When you attend each session of radiotherapy, the radiographer will carefully position you on the couch and make sure that you are comfortable. The couch is very firm but the radiographer may put rests beneath your knees or put your feet into rests to make it more comfortable and to help you remain still. The treatment usually lasts only a few minutes and you will be alone in the room during this time. You will be able to talk to the radiographers should you need to as they will be monitoring you closely from the next room.
External radiotherapy is not painful but you do need to lie still when the treatment is being given. The radiation machine may move round you but doesn’t touch you. The radiotherapy treatment will not make you radioactive and it is perfectly safe for you to be around other people, including children, after your treatment. Always make sure that you drink plenty of water throughout the entire planned timescale for your radiotherapy treatment and especially make sure that you have a full bladder during each treatment as this helps to protect the bladder.
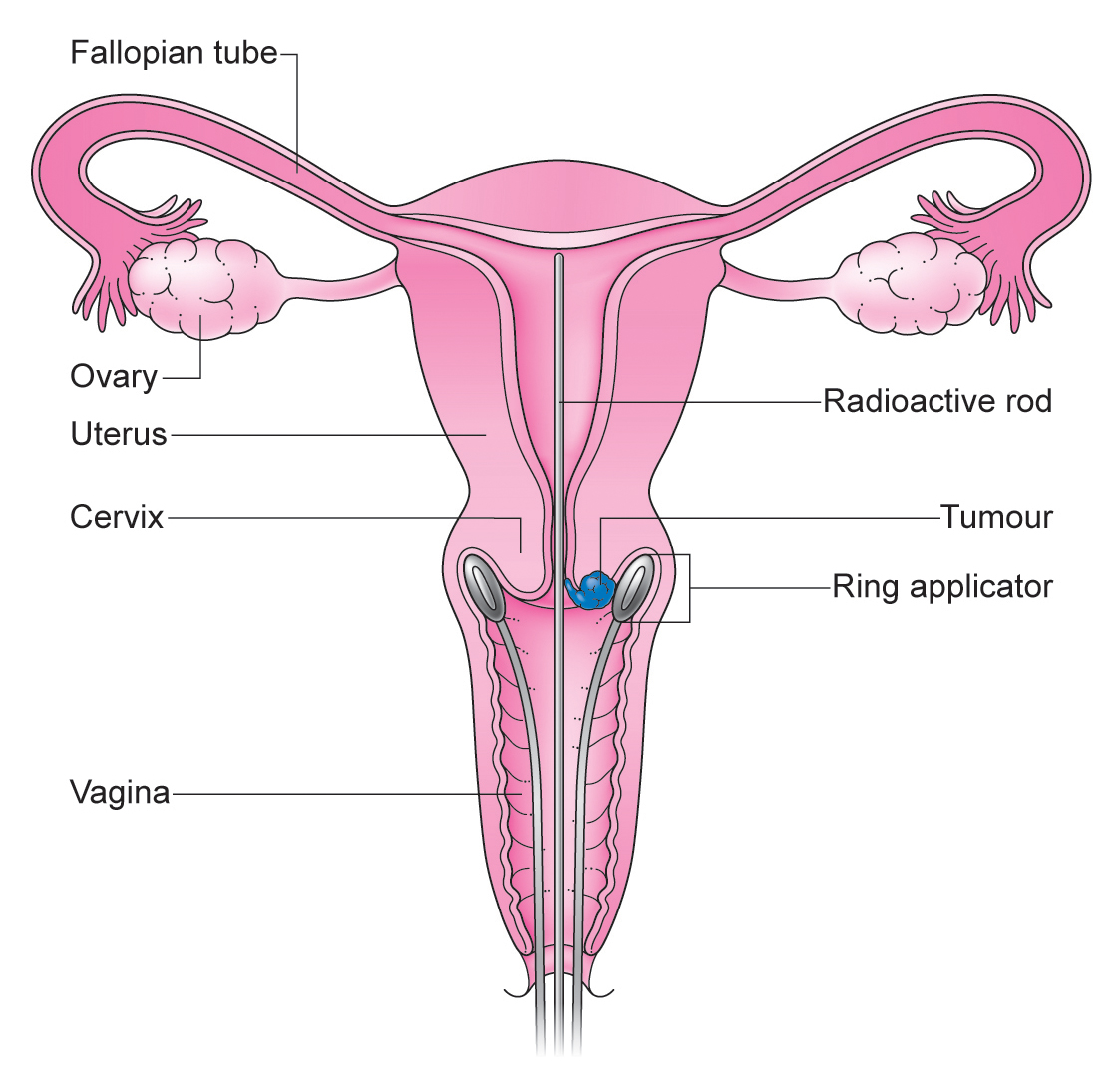
Internal Radiotherapy (Brachytherapy)
Brachytherapy gives a controlled dose of radiotherapy directly to the cervix and the areas close by. Under a general anaesthetic, tubes are places into the vagina and uterus so that the tubes lie directly touching the tumour. Radioactive balls (sources) can then be fed into the tubes and the radiation spreads directly out of the tube to the tumour. Sometimes you will have to have a scan with the tubes in place before the radiation dose is given. In some centres you will return to the ward after theatre with the tubes in place and the radiation is delivered by a machine, usually a selectron, for up to 24 hours. You will have to remain in bed during this time and will have a catheter in place to drain the bladder. This is generally put in place at the same time as the tubes so is in place when you wake up from the anaesthetic. The radioactive balls can be withdrawn regularly so that nurses can enter the room at regular intervals. It is not usually painful but may be uncomfortable and so painkillers can be given if necessary. Once the treatment is completed, the tubes will be removed by one of the doctors or nurses and this can be a bit uncomfortable. Painkillers will be given before they are removed and sometimes sedation or gas and air may be given to make it easier for you.
It is not possible to have visitors during this treatment and so it can make you feel very isolated, frightened and depressed at a time when you might want people around you. If you experience these feelings, it is important that you let the staff looking after you know. You might also find it helpful to take plenty of reading material and things to keep you occupied whilst you are in isolation. You only need to be in isolation whilst the tubes are in place. Once they have been removed, the radioactivity disappears and it is perfectly safe to be with other people.
In some radiotherapy departments, an implant containing a higher dose of radioactivity (microselectron) is used and this is only in place for a few minutes. These shorter treatments may need to be repeated several times, a few days apart, and may be given as an inpatient or an outpatient. It is often given under general anaesthetic for a short period of time. This treatment does not need a catheter to drain the bladder, however one may be needed when x-ray pictures are taken during the planning of the treatment.
Side Effects of Radiotherapy / Brachytherapy
Radiotherapy should not be painful whist it is being given to you during your treatment. You may find, however, that you do experience some side effects that begin to appear two to three weeks after the start of treatment and can come on quite gradually.
Common side effects of pelvic radiotherapy can be:
- Tiredness
- Diarrhea
- A burning sensation when passing urine (similar to cystitis)
- Passing urine more frequently than usual
- Sore skin
These side effects can range from very mild to more troublesome depending on the strength of the dose of radiotherapy, the length of your treatment and the size of the area treated. Your consultant or specialist nurse can advise you further on what to expect.
It is not unusual to have slight vaginal bleeding or discharge once radiotherapy treatment has ended. It is important to report any and all side effects to your consultant or nurse as they may be able to treat some of them with medicines.
These initial side effects should gradually disappear over the next few weeks after your treatment has finished.
After a few days of finishing treatment, many women report feeling a significant improvement with the above symptoms and the majority of side effects have settled by six weeks.
Possible Short-term Side Effects Post Radiotherapy Treatment
Tiredness
Radiotherapy can make you very tired. It is important to drink plenty of water and get as much rest as you can, especially if you have to travel a long way for treatment each day. Do not be surprised if some days you feel fine and other days, exhausted. You will also find that this tiredness will increase towards the end of treatment. If you do experience tiredness it should decrease within a couple of months of finishing your treatment.
Diarrhea or Nausea
It is important that you drink plenty of fluids and eat as healthily as possible during your treatment. If your diarrhoea is not controlled with medicines, let your doctor or nurse know. Many patients find that it can help to reduce their intake of fibre as this can impact on the severity of the diarrhoea. You may feel sick during treatment. If you don’t feel like eating, you can have nutritious high-calorie drinks instead of meals.
Burning Sensation Passing Urine
It is important during treatment to drink plenty of water and it is advised that you ensure that you have a full bladder when having external radiotherapy as this helps protect the bladder. Some patients report symptoms similar to cystitis towards the end of treatment (i.e. need to pass urine more frequently, burning sensation when passing urine, increased urgency and some urinary incontinence). Once treatment has finished, these symptoms should decrease within the first month.
Sore Skin
Your skin may get sore in the area being treated. Perfumed soaps, creams or deodorants may irritate the skin and should not be used during the treatment. Your radiographer or nurse can advise you on skin care during this time. You may find that in the first few weeks of finishing treatment, your skin may feel worse before it improves so continuing to use products without perfume or chemicals can help to reduce these effects. You will also be advised to stay out of the sun and to avoid sunbathing. You may find that your skin is, in general, a little more sensitive for a few months after treatment.
Possible Long-term Side Effects Post Radiotherapy Treatment
Pelvic radiotherapy can sometimes lead to long-term side effects. It is generally accepted that you are likely to notice some changes in your bowel, bladder and vagina in the months and years after treatment but it will vary from person to person.
Each patient will be affected differently according to how much treatment they have received, the location of their cancer and how well their body has tolerated the treatment. For this reason, it is impossible for us to gain an overall statistic of those affected by pelvic radiotherapy and to what degree. Some women report very mild changes which do not impact on their quality of life, whilst others are greatly affected. Any persistent changes will need to be discussed with either your GP or at follow up appointments with your oncologist. One thing that may help decrease the chances of developing side effects is to stop smoking during and after the treatment. So if you do smoke, you should try cutting down or stopping.
Menopause
Unfortunately, radiotherapy for cancer of the cervix affects the ovaries and brings on the menopause, usually about three months after the treatment starts. This means that your periods will stop and you will have menopausal side effects such as hot flushes, dry skin and possibly loss of concentration. Some women become less interested in sex and notice that their vagina is dry. Sometimes radiotherapy causes a narrowing of the vagina, which can make sexual intercourse uncomfortable.
The menopausal side effects can be reduced by taking hormone replacement treatment (HRT) as tablets or skin patches. These can be prescribed by your gynaecologist during the radiotherapy treatment or shortly after it has ended. For those wishing to opt for a more natural approach, a qualified homeopath/naturopath can advise.
Sometimes it is possible through keyhole surgery to move the ovaries outside the pelvis and try to reduce the risk of radiotherapy induced menopause but this is no guarantee that the menopause will be avoided. Your gynae-oncologist can advise you about this treatment.
Find more information about the menopause and HRT
Effects on the Bowel or Bladder
After radiotherapy, the bowel or bladder may be permanently affected. These changes can be very minor and, as such, are easily managed over time. For some women, the increase in bowel motions and diarrhoea may continue or you may need to pass urine more often than before. The blood vessels in the bowel and bladder can become more fragile after radiotherapy treatment and this can cause blood in the urine or bowel movements. Urinary or faecal urgency and incontinence can also occur in a minority of patients. This is largely caused due to the rectum and urinary tract both being close to the treatment site. Some of these effects can take many months or years to occur. These symptoms can be very distressing but, with the right attention, they can be managed with physiotherapy, dietary changes, medication, or treatment.
If you notice any of these symptoms it is very important to let your doctor know. Referral to bowel and bladder specialists is appropriate so that they can carry out specific tests to find the precise cause of the symptoms. This can lead to successful treatment to ensure quality of life is improved, if not returned to normal.
Effects on the Vagina
Radiation treatment, whether by external beam radiation or by internal radiotherapy (brachytherapy), will cause changes to the vagina such as the drying and thinning of the vaginal lining, fibrosis (formation of scar tissue), shortening and narrowing of the vagina and reduction in the amount of vaginal lubrication. It is also likely to reduce the size and number of small blood vessels within the vagina. This will lead to the tissue in the vagina to lose some of its elasticity. In the first few months after treatment finishes you may also find that you experience a change in vaginal discharge (which might also smell unpleasant). It is important to let your doctor know as it is possible that you could have an infection that will need a course of antibiotics.
After treatment, you might find that sexual intercourse is difficult or painful. Your specialist nurse will discuss with you the use of dilators and hormone creams to keep the vagina supple. It is most important to follow the nurse’s instructions on using the dilators as not only will this help allow you to continue a normal sex life with your partner (or future partner) but also ensures that you are able to be properly examined at your follow up appointments post treatment. Some women find it easier both physically and psychologically to use a vibrator instead of the dilators as this can make the process less ‘medical’.
Many women find this one of the most challenging aspects of coping with changes to life after cervical cancer, so please do ask for support from your health care team.
Lymphoedema (swelling of the leg / groin)
Some women find that the radiotherapy affects the lymph glands in the pelvic area and can cause swelling in the legs and / or groin. This is called secondary lymphoedema and is more likely if you have had surgery as well as radiotherapy. Is not possible to predict who will get lymphoedema.
It is essential that lymphoedema is correctly diagnosed and appropriately assessed. Whilst there is no cure for lymphoedema, in many cases it can be managed by one of the following:
- Skin care – to keep the skin and tissues in good condition and to prevent/reduce the risk of infection
- External support/compression – in the form of elastic compression garments to help prevent the swelling from building up in the limb
- A programme of exercise and movement – to try and maximise lymph drainage without over exertion (this would cause the swelling to worsen)
- Simple Lymphatic Drainage (SLD) – a gentle massage technique that is based on the principles of Manual Lymphatic Drainage (MLD). It involves the use of simple hand movements to try and move the swelling out of the affected area. It is designed to be carried out by patients themselves – or their relatives or carers.
If you experience any swelling and pain in the groin or legs make sure you discuss it with your health care team. Read more information on life after cancer.
Chemotherapy
[/trx_title]Chemotherapy uses anti-cancer (cytotoxic) drugs to destroy cancer cells. There are several chemotherapy drugs which can be used to treat cervical cancer. The most common of these is Cisplatin and it may be given with other chemotherapy drugs. The drugs are usually given intravenously (by injection into a vein).
It may sometimes be used before surgery or radiotherapy to shrink the cancer and to make these treatments more effective. If it is given this way it is called neo-adjuvant chemotherapy.
Chemotherapy may also be given to women whose cancer has become advanced or if the cancer has returned after radiotherapy. In this situation, your oncology team will plan the best form of treatment for you according to your current diagnosis and will be highly individual. Some of the types of chemotherapy that are sometimes used are Cisplatin, Topotecan, Carboplatin and Paclitaxel (Taxol). These are used to try to shrink and control the disease and to relieve symptoms, to prolong a good quality of life. It is always helpful to discuss this type of chemotherapy and its side effects with your consultant.
Side Effects of Chemotherapy
Chemotherapy can cause side effects which may feel slightly worse if given alongside radiotherapy. Chemotherapy can temporarily reduce the number of normal cells in your blood. When there are less healthy cells in your blood you are more likely to get an infection and you may get tired easily. During chemotherapy your blood will be tested regularly and, if necessary, you may be given antibiotics to treat any infection. Blood transfusions may be given if you become anaemic.
Some of the chemotherapy drugs that are commonly used to treat cancer of the cervix may affect the kidneys. Usually this does not cause any symptoms, but the effect can be severe and the kidneys can be permanently damaged unless the treatment is stopped. For this reason your kidney function will be checked by a blood test before each treatment. You may be asked to drink plenty of fluids, and to measure how much liquid you drink and the amount of urine you pass.
Other side effects may include tiredness, feeling sick (nausea), vomiting and hair loss, although nausea and vomiting can usually be well controlled with effective anti-sickness drugs.
There is usually very little hair loss (if any) with Cisplatin chemotherapy. With other types of chemotherapy (for example Taxol), if your hair falls out it will grow back within a few months of completing treatment.
Some chemotherapy drugs also make your mouth sore and may cause small ulcers. Regular mouthwashes are important and your nurses will show you how to do these properly. If you don’t feel like eating meals, you can supplement your diet with nutritious drinks or soups. A wide range of drinks is available and you can buy them at most chemist shops or they can be prescribed by your GP.
Although these side effects may be hard to bear at the time, they gradually disappear once your treatment is over. Your doctor or nurse can tell you what problems, if any, to expect from your treatment.
Taxol (and occasionally cisplatin) can also sometimes cause tingling or numbness in the hands and feet and, in some women, this type of chemotherapy can cause more prolonged or permanent mild nerve damage.
If you find that you are experiencing any side effects at all, do speak to one of your medical team. There are so many different ways that they can help to alleviate most them that there really is no reason to suffer in silence. It could make all the difference to how you go through treatment.
Hair Loss
There is usually very little hair loss (if any) with Cisplatin chemotherapy. However, if you are given another type of chemotherapy, such as Taxol, hair loss is a common side effect. If you do lose your hair it should grow back within three to six months of completing treatment. Your medical team will be able to talk to you about how fast this will happen and what to expect.
Hair loss can be a very difficult part of the cancer journey. You can find information about head coverings and wigs in your local cancer centre. You might want to talk to someone about how your feeling, this could be a trained therapist or alternatively you might want to join a support group in your area to meet other women who are facing the same treatment.